Executive
Science Not Politics Should Guide CDC Vaccine Decisions
A likely recommendation for lowing the age for a pneumococcal vaccine will suffer if the CDC recommends one preparation only.

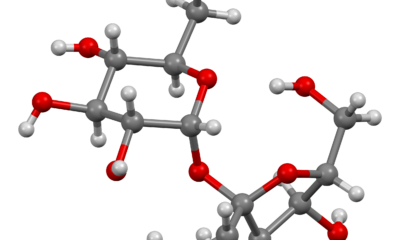
A panel at the Centers for Disease Control and Prevention (CDC) that advises the U.S. government on vaccine policy is expected to recommend lowering the age from 65 to 50 for getting a routine pneumococcal vaccination.
A lower age is fine, but why only one vaccine?
The decisions made by the Advisory Committee on Immunization Practices (ACIP) profoundly impact public health. ACIP’s recommendations dictate coverage requirements for Medicare, Medicaid, and private health plans, influencing access to life-saving vaccines for millions of Americans. For adults aged 50 and over, pneumococcal vaccines prevent severe infections like pneumonia, meningitis, and bacteremia.
However, the good science of lowering the recommended age to 50 must be combined with ACIP recommending both FDA-approved pneumonia vaccines. Any attempt to recommend only one vaccine for this age group threatens to undermine public health.
ACIP’s Role and Its Broader Implications
ACIP comprises public health experts who review scientific data to make evidence-based recommendations about the safe and effective use of vaccines. The committee advises but its recommendations must be adopted by the CDC.
ACIP’s expert consideration must not be limited to cost – public health policy must be focused on maximizing good health outcomes while offering the best possible protection for a diverse population. A singular focus on one vaccine ignores the variability in how individuals respond to vaccines, the differing side effect profiles, and the varying degrees of protection that may be needed for people with chronic conditions or compromised immune systems.
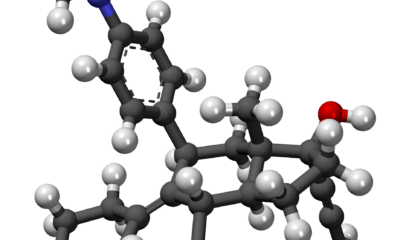
The Importance of Choice for Optimizing Immune Protection
One of the fundamental principles of vaccination is the recognition that a one-size-fits-all approach does not work for everyone. Adults aged 50 and over represent a diverse group with varying health profiles, and they may respond differently to vaccines depending on factors such as pre-existing conditions, immune system function, side effect risks, and even genetic factors.
Offering a choice of pneumococcal vaccines allows healthcare providers to choose the best option for each patient – ensuring the highest protection against severe diseases like pneumonia. Limiting access to a single vaccine could leave some individuals at greater risk of infection, hospitalization, or long-term complications, ultimately undermining the goal of public health interventions. Political pressure to choose one vaccine over another would make it impossible for ACIP to promote the tailored approach necessary to optimize immune protection.
Lessons from the 1990s: The Danger of Vaccine Shortages and Stifling Innovation
The risks of limiting choice and competition in vaccine policy are well-illustrated by the experience of pneumococcal vaccines in the 1990s. At the time, the U.S. government favored a single vaccine manufacturer to supply pneumococcal vaccines for children. This decision led to dangerous shortages, leaving many children without protection against serious infections.
This crisis revealed the dangers of creating a monopoly in the vaccine market. When competition is stifled, manufacturers have little incentive to innovate or improve upon existing vaccines. The result was a shortage of vaccines and a delay in developing more effective options. By restricting access to just one vaccine today, we risk repeating past mistakes, which could lead to shortages and prevent further advancements in pneumococcal vaccine technology.
The Risk to Public Trust
When healthcare recommendations limit choice, people may perceive that the decisions are driven by political or financial motivations rather than sound public health science. If the public believes that cost-cutting measures or external pressures, rather than evidence-based analysis, are guiding decisions, trust in the CDC and other health agencies could erode. The perception that recommendations are based on price or convenience rather than individual health needs can lead to skepticism and reduce the public’s willingness to follow those recommendations.
Conclusion
The best path forward is one that maximizes choice, encourages innovation, and prioritizes the health and safety of millions of older Americans. An ACIP recommendation to lower the age for pneumonia vaccination will help patients, and not recommending one vaccine over another will help restore goodwill lost after the pandemic.
This article was originally published by RealClearPolicy and made available via RealClearWire.
Dr. Robert Goldberg is Vice President of Research Programs at the Center for Medicine in the Public Interest.
-

 Civilization4 days ago
Civilization4 days agoWhy Europe Shouldn’t Be Upset at Trump’s Venezuelan Actions
-

 Christianity Today4 days ago
Christianity Today4 days agoSurprising Revival: Gen Z Men & Highly Educated Lead Return to Religion
-

 Executive5 days ago
Executive5 days agoWaste of the Day: Can You Hear Me Now?
-
 Civilization2 days ago
Civilization2 days agoTariffs, the Supreme Court, and the Andrew Jackson Gambit
-

 Civilization2 days ago
Civilization2 days agoWhy Europe’s Institutional Status Quo is Now a Security Risk
-

 Civilization3 days ago
Civilization3 days agoDeporting Censorship: US Targets UK Government Ally Over Free Speech
-
 Executive3 days ago
Executive3 days agoWaste of the Day: Wire Fraud, Conflicts of Interest in Connecticut
-
 Civilization3 days ago
Civilization3 days agoEpstein and the destruction of trust