Executive
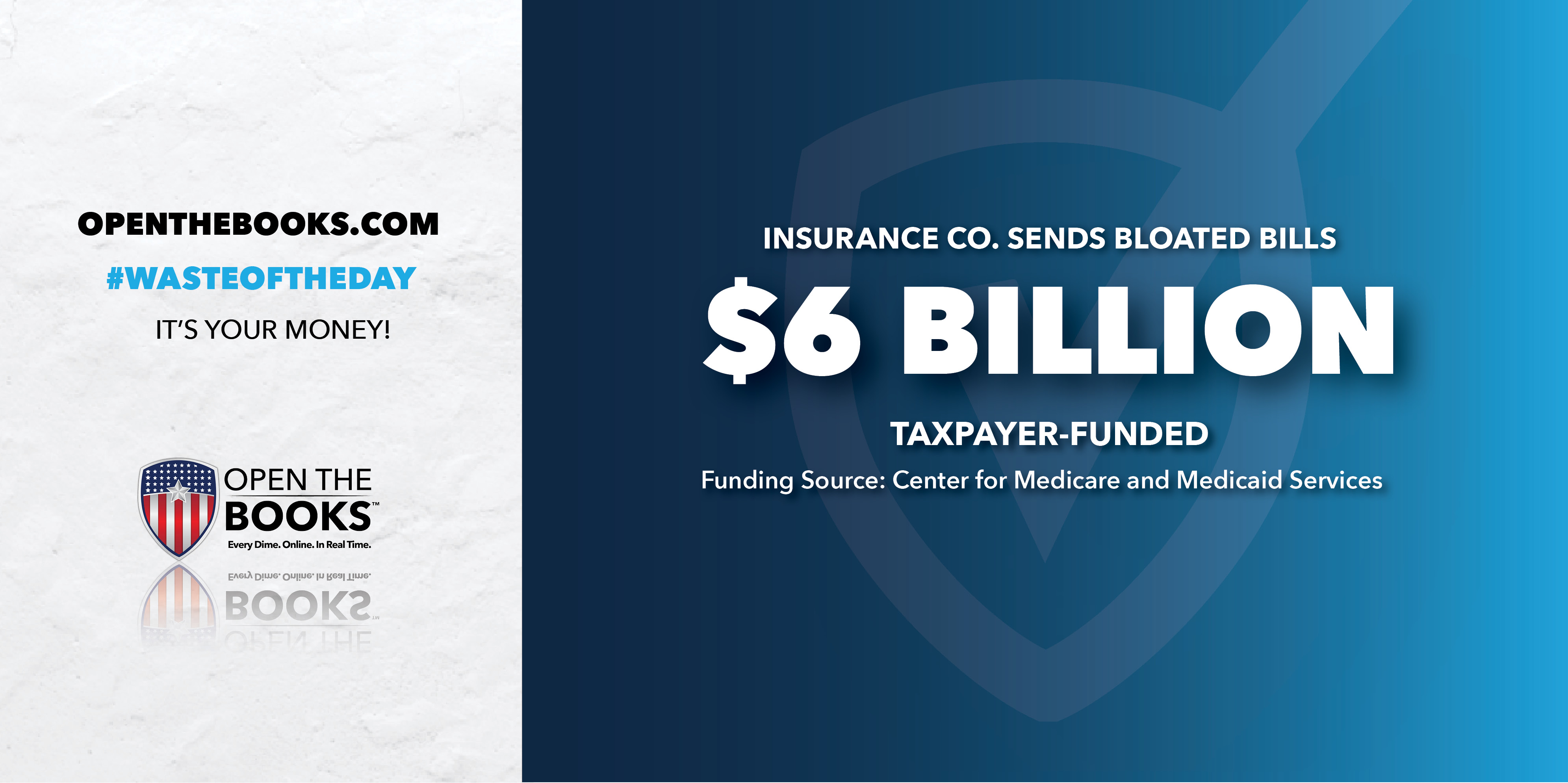
Waste of the Day: Exaggerated Medicare Diagnoses Cost Billions
United Healthcare exaggerated the state of illness of their Medicare Advantage clients, thus defrauding the government of $6 billion.

Topline: United Healthcare potentially collected an extra $6 billion from the federal government in 2023 by exaggerating how sick their patients were, according to new analysis from the nonprofit Alliance of Community Health Plans.
Medicare Advantage and how United Healthcare defrauded it
Key facts: Medicare Advantage is an alternative to traditional government-run Medicare that allows elderly patients to use private health insurance companies, which get reimbursed every month based on how many patients they cover.
Because elderly patients can be expensive for private companies to insure, the government offers “risk adjustment” payments, reimbursing the companies more money for covering patients who are very sick or have several medical problems.
Open the Books
However, the private companies are often not entirely honest with their risk adjustments. In a process known as “upcoding,” many healthcare providers list minor diagnoses that most doctors would ignore, just to make their patients appear sicker and get a higher reimbursement rate from the government. Some companies have even been caught making up medical conditions their patients don’t have.
Now, hard evidence has emerged. United Healthcare’s risk adjustment scores are 36% higher than those of local nonprofit health-care plans, according to the Alliance of Community Health Plans. That helped United, the nation’s largest Medicare Advantage provider, receive an extra $785 per patient in 2023, costing the federal government $6 billion.
Humana, the second-largest Medicare Advantage company, has risk adjustments that are 19% higher than local nonprofits, costing an extra $423 per patient.
One percent of the total damage from such fraud
Search all federal, state and local salaries and vendor spending with the world’s largest government spending database at OpenTheBooks.com.
Background: The 2023 overpayments are a small part of the damage that dishonest practices are expected to cause to Medicare Advantage.
The Committee for a Responsible Federal Budget estimates that from 2025 to 2034, the government will unnecessarily spend $600 billion because of upcoding. Medicare patients will also be overcharged an estimated $110 billion from their own money.
Medicare will also lose $580 billion because of “favorable selection,” a process where Medicare Advantage providers intentionally enroll patients who seem very sick on paper but are actually fairly healthy. That allows the insurance companies to boost their risk adjustments while spending small amounts of money on actual health care for the supposedly risky patients.
Summary: Health-care reform is never easy, but eliminating upcoding is a common-sense goal that both Democrats and Republicans should be able to agree on.
The #WasteOfTheDay is brought to you by the forensic auditors at OpenTheBooks.com.
This article was originally published by RealClearInvestigations and made available via RealClearWire.
Jeremy Portnoy, former reporting intern at Open the Books, is now a full-fledged investigative journalist at that organization. With the death of founder Adam Andrzejewki, he has taken over the Waste of the Day column.
-
 Civilization3 days ago
Civilization3 days agoVirginia redistricting – the forgotten theater
-

 Civilization4 days ago
Civilization4 days agoWhat the Political Attacks on Fetterman Reveal
-

 Civilization5 days ago
Civilization5 days agoTrump’s SOTU Speech a Win, But It’s Not Enough
-

 Clergy4 days ago
Clergy4 days agoDecapitating Amalek: Iran, Purim, and the Obligation to Act in Time
-
 Education5 hours ago
Education5 hours agoWaste of the Day: Boston’s Soccer Stadium Cost Almost Tripled
-

 Civilization3 days ago
Civilization3 days agoIran: A Humbling Reminder of the Public Square We Take for Granted
-

 Civilization5 days ago
Civilization5 days agoTop Library Advocate: Backing Drag Queen Story Hour Supports Parental Choice
-
 Executive2 days ago
Executive2 days agoWaste of the Day: Rhode Island Overtime Payments Approach $300,000








